By Barry Keate
Barry Keate, has lived with tinnitus over 40 years and has published 150+ research articles on numerous aspects of tinnitus. He is an expert on the condition and a well-known advocate for those with tinnitus.
Due to its incessant, bothersome nature, tinnitus has been linked to depression. Depression can worsen tinnitus, which in turn can worsen depression. In order to treat the depression experienced by those suffering from tinnitus, physicians will prescribe antidepressants that often make their tinnitus worse and present a host of other potential side-effects. To avoid this scenario, some tinnitus patients who experience depression use natural remedies that contain an essential amino acid that boosts the brain’s own mood-enhancing chemicals.
One reason why many tinnitus patients suffer from depression is the debilitating nature of tinnitus. This condition can be more emotionally wearying than other types of hearing issues. One clinical study showed 60% of tinnitus patients had major depression compared to 7% of those with general hearing loss but no tinnitus. (1)

Depression is modulated by serotonin, a neurotransmitter found in the human brain and gut, which transmits nerve impulses across the synapse between neurons. Often referred to as the “happiness molecule”, serotonin has a profound effect on mood. High levels of serotonin lead to a cheerful disposition and the ability to withstand everyday stress. Low levels lead to depression, lack of anger management, obsessive-compulsive disorder (OCD), and even thoughts of suicide.
L-Tryptophan for Depression and Tinnitus
Physicians routinely prescribe antidepressants for depression. These medications do not create or boost serotonin. Instead, they inhibit the absorption of serotonin after it is used to transmit information. This keeps serotonin in the synapses between neurons longer than normal and allows it to be reused. For tinnitus patients, prescribed antidepressants may worsen their tinnitus.
There is one way, and only one way, to actually increase serotonin in the brain. This is with the serotonin precursor, L-tryptophan, also sometimes referred to as tryptophan. This amino acid crosses the blood-brain barrier and metabolizes to create serotonin, melatonin and niacin within the human brain. Melatonin is also helpful for stabilizing sleep cycles and providing a good night’s rest.
L-Tryptophan is an essential amino acid. This means the body cannot produce it and it must be supplied by the diet or supplements. It is found in most protein-based foods, most notably turkey, but is also found in oats, dried dates, chickpeas, pumpkin seeds, bananas, milk, yogurt, cottage cheese, red meat, eggs, fish and poultry.
The typical diet supplies enough L-tryptophan to provide for basic metabolic requirements. However, it often fails to provide optimal brain serotonin levels. This is because L-tryptophan is the least plentiful amino acid and competes with other amino acids for transport through the blood-brain barrier. When amino acids are consumed together, L-tryptophan is at a disadvantage and often does not transport through the barrier. It should always be taken on an empty stomach to prevent it from competing with other amino acids for absorption.
Also, as we age, L-tryptophan levels decline. This leads to a spectrum of mood disorders that include irritability, stress and anxiety. More serious symptoms, such as sleep disorders, depression, aggressive behavior, even suicide, have been traced to reduced levels of tryptophan causing a decrease in serotonin levels. (2)
Boosting and balancing brain serotonin through L-tryptophan supplementation is gaining traction among some physicians who realize that many of their depressed patients have low levels of L-tryptophan. (3)
The nutritional requirement for L-tryptophan is 5 mg/kg of body weight or about 375 mg for a 170 lb person. However, many adults choose to consume much more, up to 4-5 grams/day to improve mood or sleep. The primary side effect of this dosage is drowsiness, so it is best to start taking a lower dosage until individual side effects become known. Some side effects are seen at dosages above 5 grams/day including tremors, nausea and dizziness. In rare cases, “Serotonin Syndrome” may occur. This is a very serious condition which is the result of too much serotonin stimulation. Symptoms include delirium, hyperthermia and possibly a coma. Because of this, extreme care should be taken if tryptophan is combined with prescription antidepressants.
In 1989 there was a spontaneous outbreak of a rare and deadly disease in New Mexico. The commonality among the victims of this disease was the ingestion of L-tryptophan. The FDA immediately issued a recall of all L-tryptophan on the market and outlawed its importation. It was later determined the disease was not caused by L-tryptophan but by a contaminant introduced by the manufacturer. In 2002, the FDA removed all restrictions and L-tryptophan has since been sold freely with no further problems.
5-HTP for Depression and Tinnitus
There is another supplement, closely related to L-tryptophan which can help with depression and tinnitus. 5-HTP (5-hydroxytryptophan) is part of the metabolizing process of L-tryptophan into serotonin. L-Tryptophan converts to 5-HTP which then converts to serotonin. 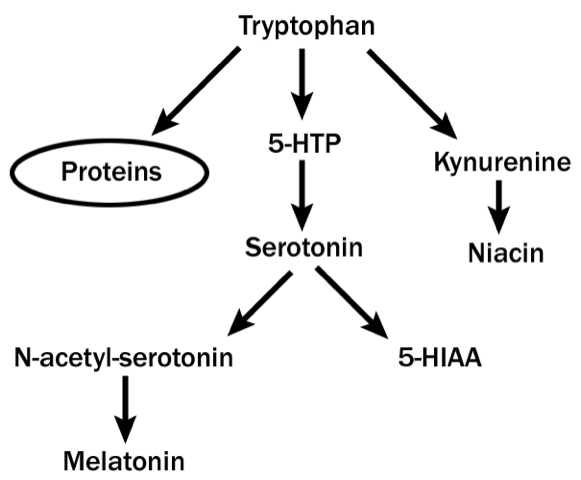
While diet can provide L-tryptophan, 5-HTP must be taken as a supplement. There has been a lot of discussion about which is the more effective product and reasons why one may be better for a given person.
5-HTP converts directly to serotonin and crosses the blood-brain barrier more easily. It is faster acting than L-tryptophan. Also, L-tryptophan competes with other amino acids while 5-HTP is better at this. Because 5-HTP is so effective, the body may build up a tolerance to it after a while.
L-Tryptophan is slower than 5-HTP but it produces better sleep. L-Tryptophan is less likely to interact with other medications and while its effects may seem subtle, it may be safer and healthier for long-term use.
The normal dosage for 5-HTP is 300 to 500 mg per day. It should be taken with food. Because it is faster acting than serotonin, it is especially important not to combine with serotonin-optimizing antidepressants.
Serotonin Optimizing Antidepressants
Prescription antidepressants are often referred to as serotonin-optimizing antidepressants. They work by optimizing existing serotonin so it is not absorbed as quickly and thus stays in the synapse longer.
There have been several generations of serotonin-optimizing antidepressants since they were first discovered accidentally in the 1950’s. The initial drugs became what is known as monoamine inhibitors (MAOI) because they inhibited the breakdown of monoamine neurotransmitters, such as serotonin, and made them more available in the brain.
There were potentially lethal dietary and drug interactions with MAOI’s and soon they were replaced by a newer class called tricyclic antidepressants (TCA). They operated along similar lines but with fewer side effects. However, side effects were still quite serious and many people could not tolerate them. The primary TCA medication is amitriptylene (Elavil), which is still in use today.
These were followed with tetracyclic antidepressants (TeCA) in the 1970’s. The most popular of these is mirtazapine (Remeron), which is widely used today. One of its most common side effects is drowsiness and it is often used for those with sleep disorders.
The newest class of these medications is what we know today as SSRI antidepressants. This is an acronym for Selective Serotonin Re-Uptake Inhibitors. These include Prozac, Paxil, Zoloft, Celexa, Lexapro and others. They are often prescribed for major depressive disorders as well as anxiety disorders, such as social anxiety, panic disorders, obsessive-compulsive disorder (OCD), eating disorders and, occasionally, post-traumatic stress disorder (PTSD).
All of these medications are synthetic. As such, thy have a host of side effects. Common side effects include nausea, drowsiness, headache, bruxism (grinding of teeth), insomnia, diarrhea, weight loss and weight gain, sexual dysfunction, increased depression, anxiety, suicidal thoughts, and tinnitus. Tinnitus is listed as a common side effect for almost all of these medications. The one antidepressant which has the lowest probability of causing tinnitus is mirtazapine (Remeron).
Furthermore, these medications have serious withdrawal problems. Because of the way these medications work, the brain is fooled into thinking that there is plenty of serotonin available and it stops making it. During withdrawal, serotonin levels drop precipitously and disturbing withdrawal symptoms which may be indistinguishable from the original illness appear. Many people who use SSRI antidepressants for long periods of time are completely unable to stop using them and are effectively sentenced to antidepressant use for the rest of their lives.
The use of prescription antidepressants is controversial, even among physicians. Two meta-analyses of clinical trials published in 2008 and 2011 found that in mild to moderate depression, the effect of SSRI’s is small or none compared to placebo. Even for severe depression, the effect is between “relatively small and substantial.” (4) (5)
Before anyone embarks on a dangerous course of prescription medications for depression, they should give considerable thought to the option of using natural L-tryptophan or 5-HTP to help with their condition. Even helping oneself to an extra serving of turkey offers more L-tryptophan.
References:
1 – Can Tinnitus be Helped with Antidepressants? Consumer Reports,
https://consumerreports.org/cro/2012/04/can-tinnitus-be-helped-with-antidepressants/
2- Sandyk R. L-Tryptophan in Neuropsychiatric Disorders: A Review. Int J Neurosci. 1992 Nov-Dec;67(1-4):127-44
3 – Sa M, Ying L, Tang AG. Simultaneous Determination of Tyrosine, Tryptophan and 5-Hydroxytryptamine in Serum of MDD Patients by High Performance Liquid Chromatography with Fluorescence Detection. Clin Chim Acta. 2012 Jun 14;43 (11-12):973-7
4 – Fournier J, DeRubeis R, et al. Antidepressant Drug Effects and Depression Severity. Journal of the American Medical Association, 303 (1): 47-53
5 – Kirsch I, Deacon BJ, et al. Initial Severity and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the Food and Drug Administration. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2253608
Get Free Shipping!
Order now and get free shipping on either the Tinnitus Starter Kit or Combo Pack. Try the doctor recommended products with clinically proven ingredients for tinnitus. No coupon code required.

