By Barry Keate
Barry Keate, has lived with tinnitus over 40 years and has published 150+ research articles on numerous aspects of tinnitus. He is an expert on the condition and a well-known advocate for those with tinnitus.
Have you ever caught yourself clenching or grinding teeth? Do you wake up in the morning with a sore jaw? You may have bruxism and it can cause tinnitus.
Bruxism is the term for the involuntary, unconscious, and excessive clenching or grinding 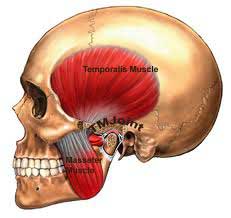 of teeth. It is one of the primary causes of Temporomandibular Joint (TMJ) Disorder, or TMD, and can lead to a host of other, unwanted side effects, including tinnitus.
of teeth. It is one of the primary causes of Temporomandibular Joint (TMJ) Disorder, or TMD, and can lead to a host of other, unwanted side effects, including tinnitus.
A previous article in this newsletter, authored by Ira Klemons, D.D.S Ph.D., discussed the incidence of tinnitus with TMD and offered several treatment therapies for the condition.
Bruxism is a habit rather than a reflex chewing activity. It can originally be caused by a number of problems, ranging from allergic reaction, medical ailments, trauma (such as a car crash), and high stress levels. Once bruxism becomes a habit, the original stimulus can be removed without ending the habit.
There are no firm figures on the frequency of bruxism because upwards of 80% of all bruxers are unaware of the habit. Children will quite frequently grind their teeth, and then grow out of it. Current estimates for the U.S. population are in the 5-20% range.
Among the numerous symptoms of bruxism are the following:
• Sore or painful jaw,
• TMJ Disorder,
• Tinnitus,
• Headache,
• Migraine,
• Blunted teeth,
• Gum recession,
• Anxiety, stress and tension,
• Depression,
• Neck pain,
• Insomnia.
As mentioned above, bruxism is one of the primary contributors to TMD. There are many other contributors. TMD is often caused by injuries that result from falls, automobile accidents, trauma at birth, etc. It is very common for the onset of symptoms to be delayed for months or years. The delay of onset occurs, in part, because these tissues progressively degenerate.
While bruxism is only one potential cause of TMD, if it is allowed to develop without treatment, it will almost always lead to the condition. About half the people who develop TMD will have tinnitus as one of the symptoms.
It is critical to get a full and accurate diagnosis. As one study states, “The average TMD patient has been seen by at least seven physicians, dentists, psychologists, or other health professionals. Of these patients, 7 out of 10 have been incompletely diagnosed or misdiagnosed.1” When TMD is found to be traceable to bruxism, it is pretty much useless to treat the TMD without addressing the underlying cause.
There are several treatment modalities for bruxism, with varying degrees of success. The most widely used treatments are detailed below.
Dental Guards and Splints
By far the most common treatment for bruxism uses the time-honored procedure of splint therapy, the use of which dates to the 1930’s. In the U.S. alone, 1.6 million splints (which may be referred to as nightguards, biteguards, occlusal splints, biteplates, removable appliances, etc.) are annually prescribed by dentists in an effort to treat bruxism.2
The dental guard or splint can reduce tooth abrasion. It protects the teeth and can reduce muscle strain by allowing the upper and lower jaw to move easily with respect to each other. This helps to reduce the bruxing pattern to avoid damage to the temporomandibular joints.
Despite the popularity of dental guards, there is significant disagreement over the efficacy of the devices. One study showed long-term reductions in symptoms of bruxism in patients who wore the splints for six months.3
Others feel that the splint does not diminish bruxing behavior over the long term, nor alleviate most symptoms and consequences. They insist that the splint may only provide a degree of protection for the teeth and a moderation of the sound in the case of those who grind.4
Author’s Note: I have personal experience that is relevant here. For two years my wife has suffered pain in her upper right cheek that she thought was related to sinus blockages or infections. After a recent CT scan by an ENT, it was determined she has TMD. The ENT conjectured she developed this from clenching her teeth as there was no wearing down of the teeth due to grinding.
On hearing this, I asked her to relax and slowly open her mouth wide. Sure enough, her lower jaw opened somewhat sideways, instead of straight up and down. This is a sign of TMD according to Murray Grossan, MD.
She was prescribed a mouth splint and has been using it while sleeping for a few months. The facial pain has completely disappeared. Fortunately, she did not develop tinnitus from the disorder.
Biofeedback
Biofeedback has long been recognized as a valuable treatment therapy for bruxism. Biofeedback entails recording signals from the sympathetic nervous system, such as heart rate, blood pressure, muscle contractions, skin temperature, etc. These signals are then fed back to the subject in the form of a computer display, alarms or other outputs. The subject can then learn to consciously control these nervous system functions over time.
signals from the sympathetic nervous system, such as heart rate, blood pressure, muscle contractions, skin temperature, etc. These signals are then fed back to the subject in the form of a computer display, alarms or other outputs. The subject can then learn to consciously control these nervous system functions over time.
Biofeedback practitioners are typically psychotherapists who hold a Ph.D. degree in psychology. Because there are many applications for biofeedback in Attention Deficit Disorder (ADD) and Attention Deficit Hyperactivity Disorder (ADHD) patients, many psychotherapists work in attention deficit clinics.
The masseter and the temporalis muscles are the two muscles used in chewing and in clenching and grinding of teeth. The masseter muscles are the primary chewing muscles and are located in front of the ear and connected to the lower jaw. It is one of the most powerful muscles in the human body. The temporalis muscles are located on the side of the skull above the ear and in front of it.
An electromyograph (EMG) is a technique for recording the electrical activity produced by muscle contractions. Measured EMG ranges are from a few microvolts up through 20 to 30 mV. When muscles contract, the electrical output increases.
EMG feedback and muscle relaxation training during the day can help patients reduce their clenching and grinding. This training will typically involve placing EMG sensors on the masseter muscle and recording the strength of contractions. When the output reaches a predetermined limit, an alarm or mild electric shock can notify the patient.
Some researchers remain unconvinced of the efficacy of daytime only biofeedback. However, the studies I found did not allow enough time for biofeedback to become fully effective. In one study, for instance, subjects undergoing daytime biofeedback for two weeks seemed to brux no less than control subjects.5 Two weeks was too short of a test period since biofeedback can take up to three months before it is fully effective for treating any disorder.
The first biofeedback headband to be worn during sleep was introduced in 2001. The headband is a battery-powered device that sounds a tone when it senses EMG muscle activity in the temporalis muscles. The tone starts off at a low volume and gets louder until the clenching stops. The intent is to allow people to stop clenching or grinding without awakening.
device that sounds a tone when it senses EMG muscle activity in the temporalis muscles. The tone starts off at a low volume and gets louder until the clenching stops. The intent is to allow people to stop clenching or grinding without awakening.
Clinical trials have shown that using biofeedback headbands after three sessions of daytime response conditioning, more than 75% of bruxism sufferers experience more than a 60% reduction in nighttime clenching from the first day of biofeedback onward. More than 50% of bruxism sufferers experience more than an 80% reduction in bruxism within the first month.6
Hypnotherapy
Bruxism is generally seen to be an unconscious mechanism to reduce stress and tension. Most people who clench or grind their teeth will state that grinding frequency increases during periods of heightened stress. Hypnosis and hypnotherapy have been shown to be effective in helping to change the unconscious mechanism that leads to bruxism.
A pilot study conducted at the Oregon Health Sciences University enrolled eight subjects with bruxism. Hypnotherapy was then employed. Both self-reports and EMG recordings were used to evaluate the therapy. The study states, “The bruxers showed a significant decrease in EMG activity; they also experienced less facial pain and their partners reported less bruxing noise immediately following treatment and after 4 to 36 months.”7
Another small hypnotherapy study showed that a 63-year old woman with a 60-year history or bruxism became symptom free after two hypnotherapy sessions. Follow-up assessments at 2, 3, and 5 years revealed that she continued to be symptom free.8
These are the only two references I could find on hypnotism and bruxism. I believe there should be much more interest and study in this field.
Dietary Supplements
Magnesium, calcium and other dietary supplements have been the subject of much conjecture and study in their relationship to bruxism. An early study, published in 1970, followed the effects of supplements on grinding and clenching. Sixteen study participants took calcium, vitamin A, vitamin C, vitamin B5 (pantothenic acid), iodine and vitamin E. When surveyed a year later, they reported their bruxism cured. A control group took only vitamins A, C, E and iodine showed no improvement. It seemed reasonable to conclude the effective ingredients were calcium and vitamin B-5.9
Another study was conducted on six patients who took, once a day, a multivitamin and multimineral tablet that contained 100 mg of magnesium, for at least 5 weeks. All patients claimed remarkable reductions, and sometimes total disappearance, in the frequency and duration of grinding. When the supplement intake stopped, the symptoms returned.10
We also have the report of a French doctor, C. Ploceniak, who has been treating bruxism with the treatment of magnesium supplements since 1980. Dr. Ploceniak claims that magnesium supplements nearly always lead to the disappearance of bruxism symptoms.11
Dr. Ploceniak treats patients with approximately 450 mg magnesium per day. Treatment must last at least 6 months, preferably a year. Some patients take longer. It is also noted that vitamin D facilitates the intake of magnesium by the body.
References
- 1- Goldman, J.R. (1992) Soft Tissue Trauma. In A.S. Kaplan & L.A. Assael (Eds). Temporomandibular Disorders (pp. 191-223). Philadelphia: Saunders.
- 2 – Pierce, C.J., Weyant, R.J., Block, H.M., Nemir, D.C. (1995). Dental splint prescription patterns: a survey. Journal of the American Dental Association. 126, 248-254.
- 3 – Sheikholeslam, A., Holmgren, K., Riise, C. (1986). A clinical and electromyographic study of the long-term effects of an occlusal splint of the temporal and masseter muscles in patients with functional disorders and nocturnal bruxism. Journal of Oral Rehabilitation 13, 137-145.
- 4 – Messing, S.G. (1992). Splint Therapy. In A.S. Kaplan & L.A. Assael. Temporomandibular Disorders (pp. 395-454). Philadelphia: Saunders.
- Pierce, C.J., Gale, E.N.(1988). A comparison of different treatments for nocturnal bruxism. Journal of Dental Research, 67, 597-601.
- “Clinical Trial Results” (http://www.StopGrinding.com/ClinicalTrials.htm).
- Clarke JH, Reynolds PJ. Suggestive hypnotherapy for nocturnal bruxism: a pilot study. Am J Clin Hypn. 1991 Apr;33(4):248-53.
- LaCrosse MB. Understanding change; five-year follow-up of brief hypnotic treatment of chronic bruxism. Am J Clin Hypn. 1994 Apr;36(4):276-81.
- Cheraskin , R. Ringsdorf, W.M. Jr. (1970). Bruxism: a nutritional problem? Dental Survey, 46 (12), 38-40.
- Lehvila, P. (1994). Bruxism and magnesium: literature review and case reports. Proceedings of the Finnish Dental Society, 70, 217-224.
- Ploceniak, C. Bruxism and magnesium, my clinical experiences since 1980. Rev Stomatol Chir Maxillofac 1990;91 Suppl 1:127.
