By Barry Keate
Barry Keate, has lived with tinnitus over 40 years and has published 150+ research articles on numerous aspects of tinnitus. He is an expert on the condition and a well-known advocate for those with tinnitus.
 The ear is divided into three parts, the outer ear, the middle ear and the inner ear. Sound collects in the outer ear, where it vibrates the ear drum. These vibrations are transmitted to the inner ear by three small bones: the malleus (hammer), the incus (anvil), and the stapes (stirrup), which increase the sound pressure and transmits the sound to the inner ear. In the inner ear, the vibrations stimulate the hair cells which transform the vibrations into electrical impulses that are carried by the hearing nerve to the brain.
The ear is divided into three parts, the outer ear, the middle ear and the inner ear. Sound collects in the outer ear, where it vibrates the ear drum. These vibrations are transmitted to the inner ear by three small bones: the malleus (hammer), the incus (anvil), and the stapes (stirrup), which increase the sound pressure and transmits the sound to the inner ear. In the inner ear, the vibrations stimulate the hair cells which transform the vibrations into electrical impulses that are carried by the hearing nerve to the brain.
If there is difficulty in the outer or middle ear, a conductive hearing impairment occurs. If the trouble is in the inner ear, sensorineural, or nerve hearing impairment is the result. When there is difficulty in both the middle and inner ear, a mixed impairment exists. Mixed impairments are common in otosclerosis but the conductive component predominates in most cases.
The primary symptom of otosclerosis is a slowly progressive hearing loss beginning anytime between the age of 15 and 45, although it usually starts around age 20. Approximately three quarters of patients with otosclerosis will also develop a ringing or rushing sound in the affected ear, also called tinnitus. In 25-30% of patients, balance problems may also occur, including unsteadiness, dizziness, vertigo, or other sensations of motion. Otosclerosis affects both ears in 80% of patients.
Otosclerosis is a common cause of hearing impairment and tinnitus, and is hereditary, although it can skip generations. About 10% of adults have otosclerosis but in only about 1% of the population does it affect the stapes, or stirrup bone where it can be detected by its interference with hearing.
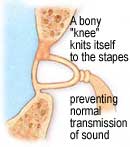
In otosclerosis, the consistency of the sound conducting bones of the ear changes from hard, mineralized bone to spongy bone tissue. This can result in a buildup of inappropriate bone around the stapes foot-plate. This buildup of bone causes the stapes to become fixed and prevents it from vibrating normally.
This type of otosclerosis is called Stapedial Otosclerosis. When otosclerosis spreads to the inner ear it’s called Cochlear Otosclerosis. Once Cochlear Otosclerosis develops, hearing impairment is permanent. On occasion, the otosclerosis may spread to the balance canals and may cause episodes of unsteadiness or dizziness.
There is no known cure for otosclerosis. However, oral fluoride supplementation may slow or halt disease progression. Dizziness associated with active otosclerosis will usually respond within two weeks of oral fluoride therapy.
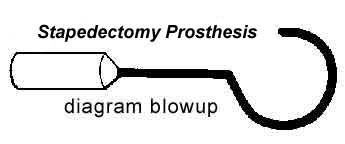
There is a stapes surgery, called Stapedectomy, which is recommended for appropriate patients. The operation is usually performed under local anesthesia and can be carried out as an outpatient procedure. Over 80% of these operations successfully improve or restore complete hearing to the patient.
In Stapedectomy, the ear drum is turned forward and the fixed stapes is removed. Tissue is placed over the opening to the inner ear and a wire, Teflon or metal prosthesis is inserted and attached to the anvil. The ear drum is then returned to its normal position and the ear canal is filled with ointment. The stapes prosthesis allows sound vibrations to again pass from the ear drum to the inner ear fluids. The hearing improvement obtained is usually permanent.
Following surgery, the use of a hearing aid on either or both ears should be considered, depending on the degree of improvement in the surgical ear. Follow up surgery on the second ear, if needed, is not performed for at least 18 months after a stable and successful result on the poorer ear is obtained.
