By Barry Keate
Barry Keate, has lived with tinnitus over 40 years and has published 150+ research articles on numerous aspects of tinnitus. He is an expert on the condition and a well-known advocate for those with tinnitus.
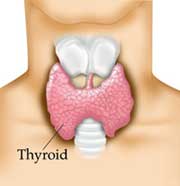 The thyroid gland is one of the largest endocrine glands in the body. It is found in the neck below the mouth. The thyroid controls how quickly the body burns energy, makes proteins and how sensitive the body is to other hormones. Dysfunction of the thyroid leads to numerous problems including lowered energy levels, increased sensitivity to pain, weight gain, depression and tinnitus. Tinnitus is a very common effect of thyroid dysfunction.
The thyroid gland is one of the largest endocrine glands in the body. It is found in the neck below the mouth. The thyroid controls how quickly the body burns energy, makes proteins and how sensitive the body is to other hormones. Dysfunction of the thyroid leads to numerous problems including lowered energy levels, increased sensitivity to pain, weight gain, depression and tinnitus. Tinnitus is a very common effect of thyroid dysfunction.
We hear from many of the people with tinnitus who suffer from a thyroid dysfunction. Tinnitus will usually reduce or resolve once the underlying problem is addressed.
The thyroid gland controls metabolism by producing thyroid hormones, principally thyroxine (T4) and triiodothyronine (T3). These hormones regulate the rate of metabolism and affect the growth and function rate of many other systems in the body. The thyroid also produces the hormone calcitonin, which plays a role in calcium absorption.
The production of T3 and T4 is regulated by thyroid-stimulating hormone (TSH) produced in the pituitary. The most common method today of determining thyroid dysfunction is the measurement of TSH.
Iodine is an essential component of both T3 and T4. T3 contains three iodine molecules while T4 contains four molecules. The vast majority of thyroid hormone produced in the thyroid gland is thyroxine (T4) which is the least active of the two. Up to 80% of T4 is converted in the liver to produce T3, which is ten times more active.
Conditions
The two most common problems in thyroid dysfunction are hormone overproduction (hyperthyroidism) and hormone underproduction (hypothyroidism).
 Hyperthyroidism is rare, affecting about 1% of the population. It results in the quickening of metabolic processes. Symptoms include nervousness, irritability, weight loss, shaky hands, panic disorder, racing heart and tinnitus. The most common cause of hyperthyroidism is Graves’ disease, an autoimmune response that over-stimulates the thyroid. The tinnitus caused by hyperthyroidism is usually associated with heart rate and is pulsatile in nature.
Hyperthyroidism is rare, affecting about 1% of the population. It results in the quickening of metabolic processes. Symptoms include nervousness, irritability, weight loss, shaky hands, panic disorder, racing heart and tinnitus. The most common cause of hyperthyroidism is Graves’ disease, an autoimmune response that over-stimulates the thyroid. The tinnitus caused by hyperthyroidism is usually associated with heart rate and is pulsatile in nature.
Hypothyroidism is much more common and may be under-diagnosed in those with less than severe symptoms. Hypothyroidism affects 1.4% to 2.0% of  women and 0.1% to 0.2% of men. The prevalence greatly increases with age, affecting 5% to 10% of women over age 50 and 1.25% of men over age 60. Typical symptoms are consistent with declining metabolic functions and range from vague complaints of fatigue to overt clinical symptoms including changes in thinking and memory, lethargy, weight gain, cold intolerance, constipation and goiterous enlargement of the thyroid gland. Other conditions such as hearing impairment and tinnitus occur, especially with the elderly. The most common cause of hypothyroidism is Hashimoto’s thyroiditis, an inflammatory condition that attacks the thyroid. With hypothyroidism tinnitus is generally present as a continuous sound.
women and 0.1% to 0.2% of men. The prevalence greatly increases with age, affecting 5% to 10% of women over age 50 and 1.25% of men over age 60. Typical symptoms are consistent with declining metabolic functions and range from vague complaints of fatigue to overt clinical symptoms including changes in thinking and memory, lethargy, weight gain, cold intolerance, constipation and goiterous enlargement of the thyroid gland. Other conditions such as hearing impairment and tinnitus occur, especially with the elderly. The most common cause of hypothyroidism is Hashimoto’s thyroiditis, an inflammatory condition that attacks the thyroid. With hypothyroidism tinnitus is generally present as a continuous sound.
Fibromyalgia and Chronic Fatigue Syndrome (CFS) are conditions frequently associated with hypothyroidism. Studies suggest that up to 15% of people diagnosed with thyroid problems will end up with fibromyalgia. It is a syndrome of chronic fatigue and diffuse muscle pain and sleep problems. It is estimated that 6 million Americans, primarily women, suffer from fibromyalgia. Chronic Fatigue Syndrome is a common problem among people with fibromyalgia, as are myofacial pain syndrome and depression.
Diagnosis
The most common test used to measure thyroid function is determination of thyroid-stimulating hormone (TSH). TSH is produced in the pituitary and stimulates the thyroid gland to secrete T3 and T4. TSH is elevated in response to low thyroid hormone levels while TSH levels are low in response to elevated thyroid hormone levels.
The standard reference range for TSH is between 0.2 and 5.5 mU/L of blood. Any reading higher than 5.5 would signal low thyroid hormone and possible hypothyroidism. Unfortunately, this range is very broad. Many clinicians and scientists believe that the upper limit in the range is far too high to permit detection in people with significantly low thyroid function.
In reality, a TSH reading of more than 2.0 may indicate lower than normal thyroid hormone levels. Patients with a reading higher than 2.0 have an increased chance of developing overt hypothyroidism and may also suffer from symptoms such as depression and weight gain.
Another complication is the fact that a patient may have perfectly normal circulating TSH levels yet still have the signs and symptoms of hypothyroidism. In the same manner that people with hyperinsulinemia become desensitized to the body’s existing insulin, these people have become resistant to T3 and T4.
Some physicians find the standard tests so unreliable they diagnose depending on symptoms. Carol Roberts, MD, Director of Wellness Works in Tampa, FL states she finds the blood tests “shockingly” unreliable and will believe the patient and her own eyes rather than the tests. She conducts the blood tests for the sake of documentation and just in case they are abnormal.
Treatment
The most common treatment for low thyroid hormone levels consists of thyroid hormone drug replacement therapy. Conventional treatment almost always begins with synthetic T4 drugs including Synthroid® or Levoxyl®. Low doses are usually used at first because a rapid increase in thyroid hormone may result in cardiac damage.
For some patients, hypothyroidism symptoms persist despite standard treatment. T4 therapy may be no more effective than placebo in improving cognitive function and psychological well-being in patients with symptoms of hypothyroidism despite thyroid tests scores well within the reference range.
For these patients, only a combination therapy, using synthetic T4 combined with T3, is able to restore natural hormone levels. One such combination drug is Thyrolar®, which combines synthetic T3 and T4 in a fixed 4:1 ratio. Caution must be used in administering T3 to people over the age of 50 because of possible cardiac problems.
In some cases hypothyroidism is accompanied by iron deficiency. When this occurs, supplementing with iron will often produce the required therapeutic results. Patients with hypothyroidism should routinely be checked for iron deficiency.
Natural thyroid medications that contain desiccated thyroid derived from the thyroid glands of the pig are also available. These medications include Armour thyroid (Thyrar®), Nathroid® and Westhroid®. Natural thyroid extracts have been used since 1892 and were approved by the Food and Drug Administration in 1939. These natural thyroid extracts were largely replaced in clinical medicine by Synthroid because doctors believe they are inconsistent from dose to dose. This, in spite of the fact they are made to standards approved by the United States Pharmacopoeia.
Patients with hypothyroidism show greater improvements in mood and brain function if they receive treatment with Armour thyroid rather than Synthroid. Researchers found that substituting Armour thyroid led to improvements in mood and in neuropsychological functioning. They are also much less expensive than the newer, patented synthetic medications.
Helpful Supplements
There are several dietary supplements that are helpful in supporting the thyroid and preventing the progression of disease.
1 – Iodine. It is extremely important to thyroid health as it is the building block of thyroid hormones. However, it is a double-edged sword as too much iodine causes or worsens the same problems as not enough.
There are many areas of the world where iodine is deficient in the soil. The area around the Great Lakes used to be known as the goiter belt because the soil is particularly iodine deficient. However, iodine deficiency was practically wiped out in the US when iodized salt was introduced. Vegetarians and vegans are at risk if they avoid salt and do not eat iodine enriched dairy products.
The likelihood that a thyroid problem is caused by iodine deficiency is a factor of geographic location, diet and the use of salt and iodized products. Most cases of thyroid dysfunction are not caused by iodine deficiency.
Recommended dosage: 150 to 300 micrograms (mcg) daily.
2 – Zinc. Animal studies show that zinc deficiency is associated with decreased serum T3 levels. Zinc may play a role in thyroid hormone metabolism in patients with low T3 and may contribute to conversion of T4 to T3 in humans. Individuals low in zinc also have an increased chance of tinnitus.
Recommended dosage: 30 to 60 mg daily.
3 – Selenium. Required for appropriate thyroid hormone synthesis, activation and metabolism. Selenium deficiency may seriously influence the generation of free radicals, the conversion of T4 to T3 and the autoimmune process.
Recommended dosage: 200 to 400 mcg daily
4 – Vitamin D. Necessary for thyroid stimulating hormone production in the pituitary gland.
Recommended dosage: 800 IU daily.
5 – Vitamin E. Antioxidant that can protect from increased oxidation and thyroid cell damage.
Recommended dosage: 400 IU daily.
6 – Vitamin C. In combination with Vitamin E reduces hypothyroidism in animals.
Recommended dosage: 2 to 3 grams daily.
